Stories
Stories
Read the stories about our work, from those who do the work, and our upcoming programs, press releases, and project highlights.
View Page: Eight Years of SAFEMed: Building a More Resilient Health System in Ukraine


Eight Years of SAFEMed: Building a More Resilient Health System in Ukraine
View Page: El modelo de atención prenatal grupal de MSH se integra en las normas de atención médica de Guatemala


El modelo de atención prenatal grupal de MSH se integra en las normas de atención médica de Guatemala
View Page: MSH’s Group Antenatal Care Model Integrated into Guatemalan Health Care Norms


MSH’s Group Antenatal Care Model Integrated into Guatemalan Health Care Norms
View Page: Eight Years of Driving Change: Voices from Ukraine’s Path to Safe and Affordable Medicines


Eight Years of Driving Change: Voices from Ukraine’s Path to Safe and Affordable Medicines
View Page: Guatemala’s Alcohol Tax Helps Advance Reproductive and Maternal Health
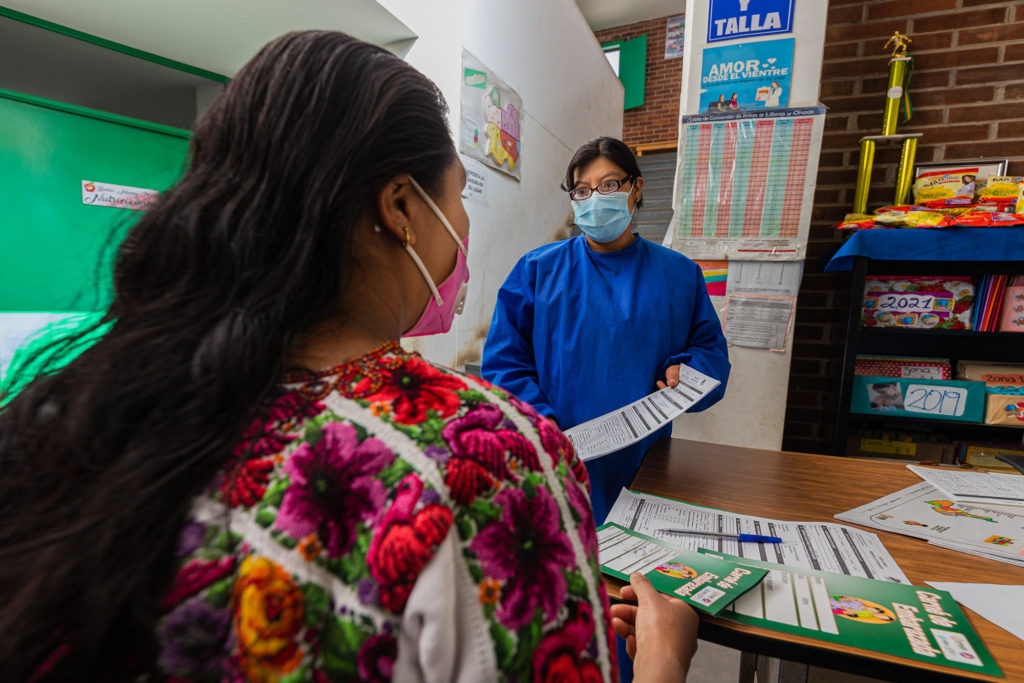
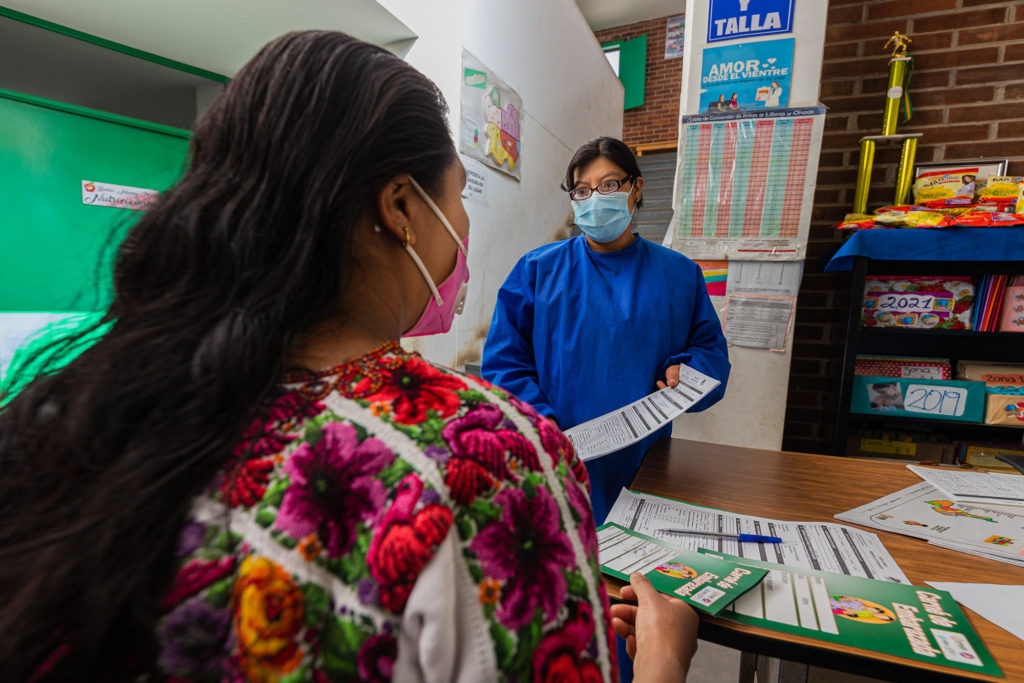
Guatemala’s Alcohol Tax Helps Advance Reproductive and Maternal Health
View Page: Locally Led, Data Driven: Ethiopia Endorses NSCA 2.0 to Institutionalize Health Supply Chain Maturity


Locally Led, Data Driven: Ethiopia Endorses NSCA 2.0 to Institutionalize Health Supply Chain Maturity
View Page: Management Sciences for Health Welcomes Dr. John Paul Clark to its Board of Directors


Management Sciences for Health Welcomes Dr. John Paul Clark to its Board of Directors
View Page: Ethiopia Advances Health Procurement Reform with Multi-Vendor Sourcing Strategy


Ethiopia Advances Health Procurement Reform with Multi-Vendor Sourcing Strategy
View Page: Innovation in Motion: SAPICS 2025 and the Future of Supply Chains


Innovation in Motion: SAPICS 2025 and the Future of Supply Chains
View Page: Stronger Planning, Stronger Access: SCS Supports Ethiopia’s Health Commodity Supply Review


Stronger Planning, Stronger Access: SCS Supports Ethiopia’s Health Commodity Supply Review
View Page: Stronger Primary Health Care, Healthier Communities: How Local Leaders Are Driving Change


Stronger Primary Health Care, Healthier Communities: How Local Leaders Are Driving Change
View Page: Strengthening Leadership for Emergency Preparedness: New Insights from Six Countries

