Our People
Our People
MSH’s team consists of a global body of people passionate about making quality health care available for all. The backbone of our work is our worldwide technical expertise across the whole health system, guided by a Leadership Team and Board of Directors committed to our mission.

Regine Alexandra Emilien
Senior Principal Technical Advisor, Local Capacity Strengthening

René Berger
Senior Technical Director and Practice Area Lead for Pharmaceutical Systems Strengthening and Supply Chain Systems

Amy Boldosser-Boesch
Senior Technical Director and Practice Area Lead for Health Policy, Advocacy, and Engagement and Integrated Health Care

Jane Briggs
Senior Principal Technical Advisor, MTaPS Program, Maternal, Newborn, and Child Health

Andrew Brown
Senior Principal Technical Advisor, MTaPS Program, Governance and Capacity Development
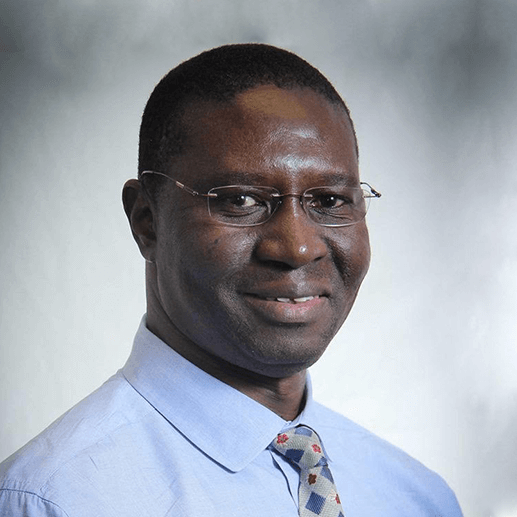
Seydou Doumbia
Technical Strategy Lead, MTaPS Program, Francophone Africa

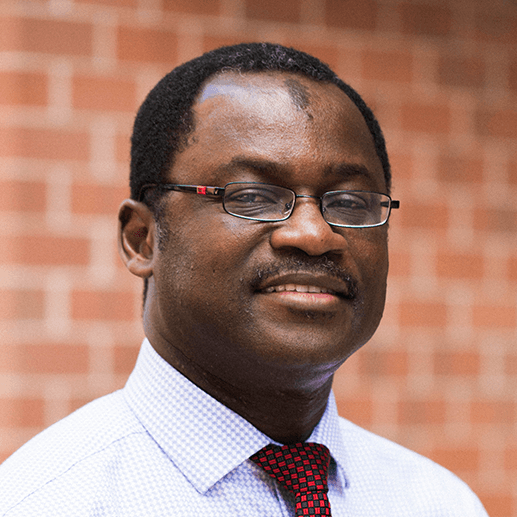
Olumide Elegbe
Director, Strategy, Business Development, and Partnerships

Colin Gilmartin
Principal Technical Advisor, Health Economics and Financing

Tamara Hafner
Senior Principal Technical Advisor, MTaPS Program, Research
For More Information on Our Programs and Technical Experts
Please direct all inquiries and media or speaking engagement requests for our Technical Experts to Jordan Coriza at jcoriza@msh.org or 617-250-9107.